Three Simple Steps Towards Cervical Cancer Prevention
Cervix is an integral part of the reproductive system. It is the opening to the womb (uterus). Cervical cancer manifests as a cancerous growth inside the cervix. It may take several years for a pre-cancerous lesion to turn into cancer of the cervix and sometimes they may never transform into malignant lesions. It may not cause any symptoms until it has advanced. In advanced stages, it may manifest as abnormal bleeding, discharge from the vagina, pain during intercourse, etc.
In India, cervical cancer is the second leading cause of cancer. In spite of its notorious reputation, cervical cancer can be prevented or managed easily with the following prevention strategies. Every woman must learn these simple steps she can take towards cervical cancer prevention.
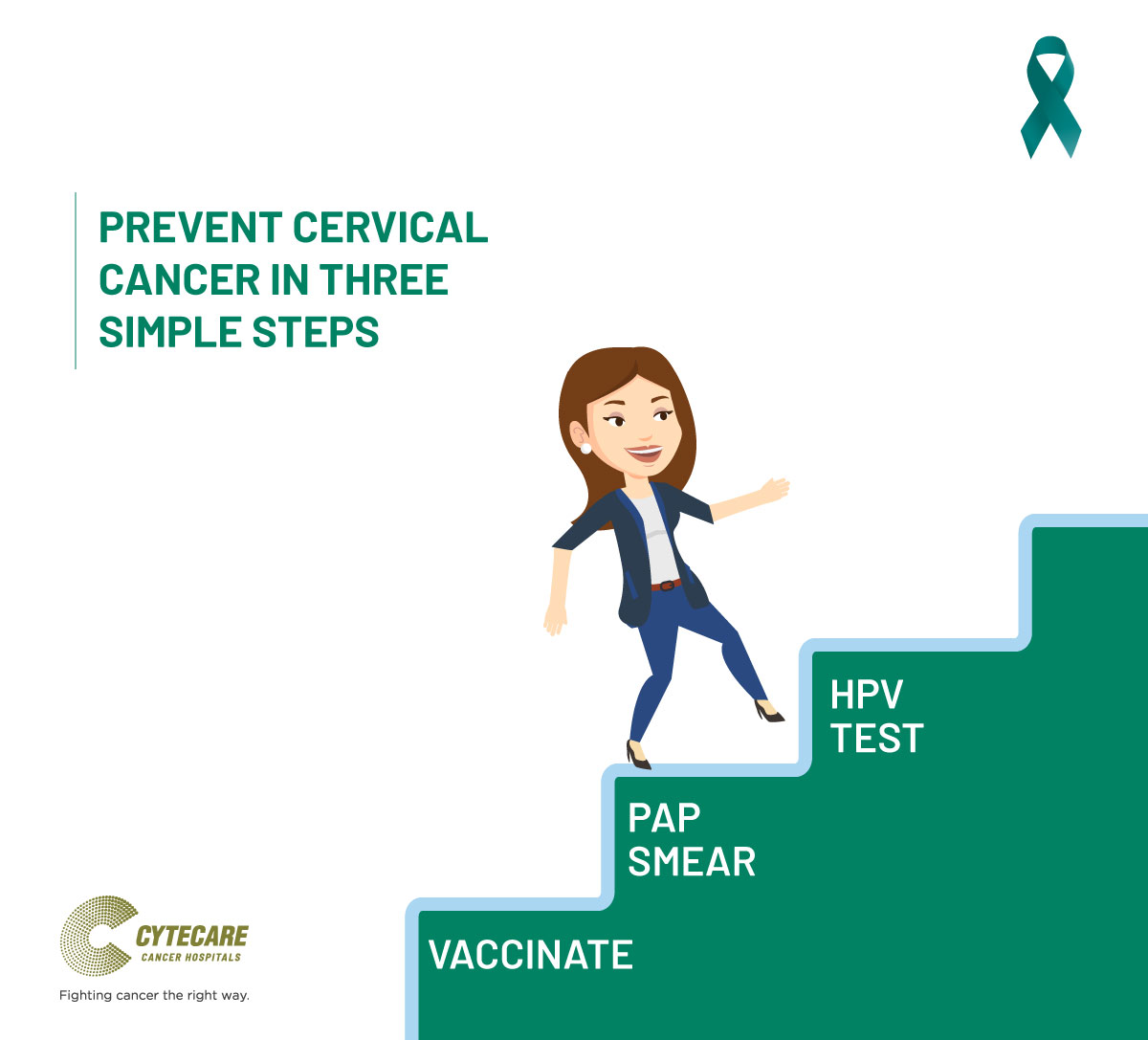
Here are the 3 Simple Steps For Cervical Cancer Prevention:
-
Cervical Cancer Vaccination
Human Papilloma Virus (HPV) is a non-enveloped DNA virus. Over 100 serotypes of HPV have been discovered, however, serotype 16 and 18 contribute the highest towards cervical tumour development. HPV infection may cause morphological changes to cervical cells that may below-grade or high-grade lesions (cervical intraepithelial neoplasia CIN1, CIN2, CIN3) and subsequently invasive cervical cancer (ICC).
Cervical cancer often strikes at the productive period of a women’s life. It is estimated that more than 80% of sexually active women acquire genital HPV by age 50. Hence, with the availability of two HPV vaccines, prevention through vaccination seems to be an effective strategy for cervical cancer.
Prevention of genital HPV infection is not possible without abstinence. Data shows that adherence to Routine Pap tests still continues to be non-satisfactory, especially in a large population like India. Hence, Vaccination is one of the best forms of cervical cancer prevention. The HPV vaccines are recombinant vaccines, two licensed vaccines are available for use in India namely- Cervarix™ and Gardasil™. Gardasil™ protects against both genital warts and cervical cancer, unlike Cervarix™ which confers protection only against cervical cancer. It is important to note that these two vaccines are prophylactic and not therapeutic.
The HPV vaccine has not yet made its way into the compulsory vaccination and remains an optional choice for a woman to make. It is a 0.5mL dose, given intramuscularly. Girls in the age group of 9-12 years must be vaccinated. Booster doses are recommended at months 2 and 6 for Gardasil™ and months 1 and 6 for Cervarix™ from the initial vaccination month.
In 4% of vaccination, minor side effects such as fever may develop. A catch-up vaccination can be given until age 26 and not more. People allergic to yeast, pregnant women, may be contraindicated to take this vaccine. At the moment the high cost of the vaccine has been the bottleneck in large-scale immunization, but until a low-cost public vaccination program is drawn out in India, this may prove as the best option considering the cost and psychological burden of cervical cancer treatment otherwise. A Routine Pap test seems to be the next best alternative.
-
Take The Pap Test
The Pap test is a screening test for cervical cancer. The test looks for abnormal cells in your cervix that could possibly turn cancerous over time. This test allows for identifying lesions that have a possibility to turn cancerous and can be monitored or treated as appropriate.
It is recommended that women between the ages of 21 to 65, must undergo regular Pap smear tests. Women with normal Pap test results need to repeat the test once every 3 years. Your Pap results may be “Normal”, “Unclear”, or “Abnormal”. An abnormal result may be described as high-grade or low-grade depending on the abnormal cellular changes observed in the cervical cells. The high-grade changes need more careful monitoring and action. These may be also termed pre-cancerous.
-
Get the HPV Test when recommended
The human papillomavirus is known to cause many conditions such as genital warts, respiratory papillomatosis, etc. However, HPV type 16 and 18 contribute to 70% of all cervical cancers worldwide (41-67% of high-grade lesions & 16-32% of low-grade lesions). Besides HPV16/18 other strains such as 31, 33, 35, 45, 52, and 58 also contribute to about 20% of cervical cancer. Hence, an HPV test is aimed at identifying the type of virus that is linked to cervical cancer.
An HPV test checks for the presence of viral DNA in the cervical cells. It is usually recommended for women age 30 and above along with the PAP test. This is called HPV co-testing. An HPV test result will usually stated as “Negative” or “Positive”. A Positive test result indicates that you have an HPV that is linked to cervical cancer. Both the Pap and HPV test results are used to make a decision regarding the next steps.
If your Pap test and HPV test both are negative, you will be asked to repeat the tests after 5 years. If your test is normal, but you tested positive for HPV, it is possible that your immune system may fight off the HPV, however, you will be recommended to repeat a PAP every year and careful monitoring may be needed.
If you have an HPV, but your Pap test is Unclear, then your physician may take a closer look at your cervix using colposcopy and may choose to remove the abnormal cells or lesion or may just monitor carefully. If both the Pap as well as HPV test show positive, then depending on the grade or severity of the lesion, the lesion may be biopsied and treated as appropriate.
Your responsibility towards Cervical cancer prevention does not end with these three steps. It is important to also maintain a healthy lifestyle. Your conscious actions such as staying away from smoking, alcohol, consuming Fiber-rich balanced diet with fruits and vegetables, and moderate-intensity exercise on a daily basis can play a role in boosting your immunity and fighting off HPV. A concerted effort in spreading awareness as well as following the recommended guidelines for screening can help reduce the risk of Cervical Cancer and its burden among Indian women.